Any trauma to the hand and wrist, even the most benign in appearance, very often following a fall on the heel of the hand, is likely in the short, medium and long term to leave sequelae. painful and stiffening capable of having a considerable impact not only in professional or sporting life (cycling, racket sports, ball sports, combat sports, etc.) but also in everyday life. This should encourage the traumatized to consult as soon as possible with the agreement of his attending physician. (without going through a general emergency service), a specialized orthopedic service SOS Main because the management of these traumas or micro-traumas is unique and requires very specific skills and know-how. If there is one lesion that should not be overlooked until radiological proof to the contrary, it is the fracture of the scaphoid bone of the wrist and three other lesions, also benign in appearance, but just as heavy with consequences: the scapholunate and to a lesser degree pyramido-lunar sprains, by rupture of one or the other of the two intrinsic ligaments of the 1st row of the carpus, but also the disintegration of the triangular ligament of the wrist on its ulnar side (internal ).
The wrist
It is delimited at the top by the lower end of the forearm and at the bottom by the base of the 5 metacarpals and wedistinguish 2 joints: the radio and the medio carpal. On the wrist many tendons are inserted, while others only cross it to go on the hand.
The hand
It consists of:
1- of 4 types of articulation: the metacarpophalangeal (AMP), the proximal (IPP) and distal (IPD) interphalangeal and the trapezio metacarpal for the thumb. These different joints are stabilized laterally by collateral ligaments and on the front by the palmar plate at the base of the first two phalanges.
2- an intrinsic musculature:- lumbricals- interosseous
- thenar muscles for thumb mobility
- hypothenar muscles for the mobility of the 5th finger.
3- an extrinsic musculature for the flexion and extension of the fingers and extrinsic tendons sliding in fibrous sheaths.
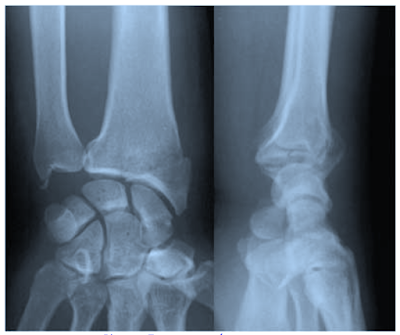
1/ SCAPHOID FRACTURESThe Scaphoid, a very poorly vascularized bone, is tied by ligaments going from the radius to the large bone and which hook the fracture hindering its consolidation.
The Scaphoid fracture must be evoked in principle in an athlete (combat sports, team sports, imbalance and fall from bicycle and motorcycle) in the face of any wrist trauma with fall on the heel of the hand, wrist in extension resulting in a swollen wrist on its lateral and painful side and without waiting for radiological confirmation which can sometimes be delayed until the 30th day (do not hesitate to ask for a CT scan or an ultrasound).
After icing and immobilization in a pressure dressing, the injured person must be referred to an SOS Hand service, especially if 3 very suggestive signs of fracture are present:
1- the pain caused by the pressure of the anatomical snuffbox.
2- painful telescoping of the thumb column.
3- painful palpation of the anterior tubercle of the S. on the palmar side of the wrist.
The 4 x-ray views of Schneck which unroll the scaphoid will specify the seat of the fracture: neck, upper or lower pole; the horizontal, oblique or vertical fracture line and the extent of the displacement. Be careful on the front X-ray, you can't see the fracture.
If the lesion is stable, it will be treated orthopedically by immobilization in plaster for at least 3 months, which will take the elbow for the first 45 days.
Unstable fractures will benefit from surgical screwing in compression with a Herbert screw.
The disappointing treatment of scaphoid pseudarthrosis is the complication to be feared in the event of delayed diagnosis or inappropriate management in a non-specialized environment.
There is also the possibility of associated ligament lesions (scapho or pyramido-lunar) with a fracture of the scaphoid with potential destabilization of the carpus.
scaphoid pseudarthrosis
compression screwing of the scaphoid with a Herbert screw
Note to the reader: we advise, for more complete information, to read the article of the blog devoted specifically to fractures and pseudarthroses of the scaphoid. NB: what clinically comes closest to a scaphoid fracture is an undisplaced articular fracture of the styloid process of the radius (external cuneal fracture) of orthopedic treatment. Anatomically the two lesions are very close and all three examination signs of a scaphoid fracture: exquisite pain at the bottom of the anatomical snuff box, pressure from the anterior tubercle, and telescoping of the thumb column are present in a cuneal fracture outside of the wrist. But if we shift the pressure point a little upwards, we also trigger an exquisite pain on the styloid process and it is finally the imaging (x-rays and scanner if the fracture line is not very clear) who will specify the lesion and dictate the action to be taken.external cunean fractures: the fracture line detaches the radial styloid, the displacement of which is often small. 2/ INTRINSIC SPRAINS (scapholunate, pyramido-lunar, triangular ligament) OF THE WRIST
Intrinsic sprains of the wrist constitute a diagnosis of elimination (above all think of a fracture of the SCAPHOID+++ which is sometimes associated with an intrinsic sprain). The lesional mechanism is that of a fall on the palm of the hand with the wrist in hyperextension. Imaging (x-rays and arthrography) is essential for diagnosis.
The most frequent and the most serious, because quickly arthrogenic, of the intrinsic sprains of the wrist is the Scapho - Lunar sprain: the wrist is swollen, the pain is dorsal and lateral with a feeling of instability and jerkiness when it is mobilized : sign of "sloshing" and Watson's test ( this test is carried out by exerting pressure on the palmar surface of the distal pole of the scaphoid and by putting the hand in radial inclination. Normally the scaphoid flexes in radial inclination. By doing this test this movement is blocked and a painful jump is reproduced because the flexion of the scaphoid occurs suddenly at the end of the maneuver ). Frontal X-rays show a scapholunate gap greater than 3 mm with horizontalization of the scaphoid; in profile the Semi Lunar is tilted back in DISI. Arthrography visualizes the ligament lesion.
The other clinical form is the Luno-Pyramidal sprain with forward tilt in VISI of the Semi-Lunate on the profile x-rays of the wrist. To behave
Faced with a swollen, painful and unstable wrist, it is best to refer the injured person to a hospital or private SOS Hand service which will take care of this acutely painful wrist in the most appropriate way, with the prior demonstration of the lesion by an arthro-scan which is the most efficient examination or better by an exploratory arthroscopy++.
Acute treatment is a matter for a hyperspecialized surgeon++ and will consist either of placing a cast immobilization for 6 weeks, or surgically suturing the lesion depending on the personal data of the sedentary patient, active subject, manual worker, high-level athlete level.
Attention, it should be known that in the event of diagnostic delay, the late treatment of a chronic instability of the wrist is disappointing+++; also as quickly as possible after 1 wrist trauma, do not hesitate to consult a specialized surgeon and perform an exploratory arthroscopy+++ which will visualize one or more intrinsic ligament lesions of the wrist and will be followed by ligament repair +++ which will then have the greatest chance of success. In conclusion: For Didier Fontès, only early and appropriate management of these lesions allows optimal restitution of the traumatized wrist to be envisaged. A specialized clinical examination, an in-depth radiographic assessment (usually an arthro-scanner) and often the earliest surgical treatment are the best guarantees of a satisfactory functional result. The more advanced the stage of the lesion, the heavier the treatment: pinning under arthroscopy may be indicated in the forms seen early, but scaphoidectomy and partial arthrodesis may prove necessary, sources of sequelae which, most of the time, could have been avoided by early diagnosis and appropriate treatment.Triangular ligament sprain
The lesional mechanism of an isolated traumatic disinsertion of the triangular ligament of the wrist is most often a fall backwards on the heel of the hand positioned in pronation and ulnar inclination. Its clinical manifestation corresponds to a discreetly swollen and painful wrist on its ulnar side and sometimes unstable accompanied by snapping. Even if the trauma appears to be insignificant, you must hurry to send it to a specialized SOS Main surgeon, so much its diagnosis, which is specifically based on exploration by arthroscopy, and its therapeutic management require in-depth knowledge that only a specialized orthopedic surgeon is able to master perfectly.
The diagnosis
As indicated in the preamble, the diagnosis of an isolated attack of the triangular ligament is a matter for hyperspecialized surgeons because the structure of the TFCC is so complex and the therapeutic possibilities differ depending on whether the injured area is well or poorly vascularized, i.e. say with or without the possibility of scarring.
In acute the injured presents with a slightly swollen wrist on its internal ulnar side secondary to a fall back on the heel of the hand positioned in pronation and ulnar inclination+++. Gentle mobilization at the end of pronation and passive supination, elbow locked at 90° is sensitive, as is ulnar tilting of the hand in hyperpronation. Anterior palpation of the ulnar side is accompanied by exquisite pain which should alert the examiner.
If these 3 signs are positive, the injured person must be referred to a specialized structure without delay, taking care beforehand to freeze this traumatic wrist and immobilize it in a splint in a neutral functional position.
However, it is arthroscopy in well-trained hands that remains the most effective exploratory examination with maximum sensitivity and specificity of 100%; it alone makes it possible to appreciate the elasticity of the articular disc and the foveal disinsertions which are generally underestimated by radiological explorations.
The therapy will be:
- or medical if the perforation is of degenerative origin or due to a simple internal disturbance: temporary immobilization with a heat-formed splint, anti-inflammatory medications, physiotherapy.
- or surgery for ligament repair targeted by arthroscopic means with optical magnification which allows precise gestures and the possibility of associating an osteotomy gesture for shortening of the ulna if necessary with, as always, the informed consent of the injured party. Surgery followed by cryotherapy in the immediate postoperative period and early passive mobilization.
NB: in the event of postoperative evolution which is not quickly favorable (persistence of pain, tingling, clicking, call the surgeon again who will either reassure the patient or proceed to an additional procedure++++. Without delay do not hesitate in the face of a painful post-traumatic wrist to do an exploratory arthroscopy+++ which will visualize one or more intrinsic ligament lesions of the wrist and will be followed by ligament repair which will then have the greatest chance of success+++.
We recommend reading these 2 other blog posts in addition:
1- focus on intrinsic scapholunate and pyramido-lunar sprains of the wrist .
2- traumatic disinsertion of the triangular ligament of the wrist . 3/ WRIST TENDINOPATHIESThe tendons are numerous at the level of the wrist; they are mostly slender and they have a long, angled ride; they slide in osteo-fibrous tunnels via synovial sheaths. Tendonitis and teno-synovitis are constantly increasing and are related to hyper-solicitation of the wrist and hand caused by sports practice and leisure activities. However, a certain number of them are commonly encountered and are not characteristic of sporting activity. Others are really linked to the sporting gesture. These tendinopathies of the wrist affect either the tendon or its synovial sheath and the bursae. The origin is sometimes metabolic, but most often it is micro-traumatic by overexertion of the wrist on formations we have said are fragile, with contributing factors such as age (around 40) and quantitative and qualitative dys-training. These lesions preferably affect amateur athletes. The clinical signs are limited to localized pain most often on one of the compartments of the back of the hand (extensor tendons ++) triggered by movement, more rarely on the anterior tendons.
Examination found localized impasto and the symptomatic triad of any tendinopathy: pain on isometric resisted contraction, on stretching and on palpation. Functional impotence is variable (in athletes there is often a drop in strength of the plug). The positive diagnosis is constituted by the anesthetic test which makes the pain disappear; then it is necessary to eliminate the associated causes.
These are benign conditions and healing can be spontaneous if the deleterious sporting gesture is stopped. It is sometimes necessary to perform one or more infiltrations and correct the technical defect. In some cases the MTP (deep transverse massage) is the key to the problem.
The differential diagnosis with the help of complementary examinations (X-rays, ultrasound, MRI or arthro-scanner) is all the pathology of the hand:
- hydroxy enthesopathy - anterior ulnar calcium apatite
- infectious tenosynovitis caused by staphylococcus or even Koch's bacillus
- sequelae of old and unknown traumas on the triangular ligament and the posterior ulnar tendon at the origin of local conflict
- tunnel syndromes and EMG on partial fractures of 1 carpal bone
- occult synovial cysts of the wrist
- beginning scapho or pyramido-lunar instability
- fractures of the unciform apophysis of the hooked bone and tendinopathy of the flexor of the 5th finger and the flexor digitorum brevis.
a/ DE QUERVAIN's tenosynovitis of the 1st compartment of the wrist.
It is a pathology that affects racket athletes and those practicing rowing, skiing, fencing, tennis, gymnastics, weightlifting, kayaking.
This is a stenosing condition affecting the tendons of the 1st compartment of the wrist, the long abductor and the short extensor of the thumb, next to the anatomical snuffbox by local overexertion in repeated inclinations of the wrist.
Clinic: swelling of the external edge of the anatomical snuff box; Finkelstein's sign (thumb folded under the fingers + ulnar inclination); thwarted thumb extension with proximal pain.Imaging: X-rays and Ultrasound++ show a thickened tendon and sheath. Treatment: local infiltration of a corticosteroid.
De Quervain's T. is often associated with WARTEMBERG's neuritis which is a neuropathy of the sensory branch of the Radial nerve which emerges 9.5 cm from the radial styloid on the outer edge of the forearm with Tinel's sign at this level, dysaesthesia of the external edge which can be masked by pain from tendinopathy and sensory disturbances when touching the dorsal surface of the thumb and the 1st commissure.
Treatment of Wartemberg neuritis:
Resting splint which must avoid any nerve compression + infiltration.
In the event of failure: neurolysis of nerve compression (high frequency of anatomical variations in this region experienced by specialized SOS Main surgeons).
Wartemberg's neuritis
b/ The other dorsal Tendinopathies of the wrist
- the tendinopathy of the Radials of the 2 nd compartment:the pain is more distal on the column of the thumb at 3 finger widths from the styloid: it is the crossing syndrome or crackling ouch.
- the tendinopathy of the 3rd compartment of the long extensor of the thumb.
- tendinopathy of the 4th compartment of the proper extensor II.
- the tendinopathy of the 5th compartment of the proper extensor of the V are more anecdotal with often muscular anomalies on the 4th and the 5th compartment.
- tendinopathy of the 6th compartment of the posterior ulnar (it is an epicondylar muscle) by insertion enthesitis on the styloid of the 5th Metacarpal. Sometimes it can be in the tennis player a rupture of the internal partition of the 6th compartment after sudden movement of the wrist, pain on the ulnar styloid and sometimes not always obvious snap of the dislocation of the released tendon.
4/ FRACTURES OF THE BASE OF THE FIRST METACARPThe fractures of the base of the 1st metacarpus all occur on the same lesion mode: a mechanism of hyper abduction and hyper extension of the column of the thumb.
As in most hand and wrist traumas, they must be taken care of in a specialized service such as SOS Main, otherwise there may be functional complications at the level of the 1st commissure with type of fixation in closure given the adduction position of the wrist. distal fragment with repercussions on the thumb index pliers and fine grips. Possibility also of late degenerative complications such as post traumatic rhizarthrosis.
Clinicallythey present in the form of a painful swelling of the column of the thumb often positioned in adduction. Depending on the location of the fracture line (face and profile X-rays), we distinguish:
- extra-articular fractures whose stable forms will be treated orthopedically after reduction by plaster immobilization in the functional position with opening of the 1st commissure. - intra-articular fractures1- of ROLANDO |
ROLANDO fracture
|
2 - of BENNET which carries the medial edge of the metacarpal head.These are actually fractures - subluxations (the dislocation being linked to the traction exerted by the abductor pollicis longus and thenar muscles).
Bennet's and Rolando's fractures are treated surgically after reduction, either closed with pins, or open with immobilization for 45 days postoperatively.
BENNET fracture
5/ METACARPAL FRACTURES OF LONG FINGERS
In this type of fracture, the lesional mechanism is that of a direct impact and the most exposed sport remains boxing on the mobile metacarpals (4th and 5th metacarpus).
On the biomechanical level , the mobilities differ: the 2nd and 3rd metacarpus are fixed, the 4th is semi-mobile and the 5th metacarpal is mobile and when closing the hand, the pulps of the different fingers converge towards the tubercle of the scaphoid. This biomechanical particularity must be respected when making the therapeutic decision, which should only be made in a specialized environment (SOS Main). and mobilization and painful compression.
The diagnosis of certainty is given by x-rays which will specify the seat (base, diaphysis, neck, head) and displacement.
Treatment is a matter for specialists and will be either orthopedic or surgical, depending on the location of the fracture and the displacement, knowing that immobilization for more than 4 weeks would be detrimental to good functional recovery, even if the radiographic bone callus is still late.
6/ SPRAINS OF THE INTERNAL COLLATERAL LIGAMENT (LLI) OF THE MPA (METACARPO-PHALANGEAL JOINT) OF THE THUMBSevere sprain of the LLI of the AMP by lesional mechanism in forced abduction of the thumb, in addition to being one of the most frequent traumatic lesions of the column of the thumb (rugby, handball, volleyball, skiing) presents the particularity when the ligament main is broken from not being able to heal due to the proximity of the aponeurotic lamina of the Adductor pollicis which covers the LLI and interposes, preventing it from healing (Stener's lesion).
Mechanism of injury in forced thumb abduction
Stener lesion (interposition of the adductor pollicis)
The diagnosis of clinical severity (testing for laxity is to be avoided because it risks aggravating any bone tearing) consists of having the injured person grasp and lift a large volume object, such as a bottle, which he is incapable of to do, the AMP not being stable and the 1st commissure not being able to open well. The other signs are the perception by the injured person of a crack followed by the impression of dislocation of the AMP.
The radiographic assessment will look for any bone tearing.
Treatment: the use of an SOS Main service is essential.
A benign lesion will be immobilized for 15 days + 15 additional days for rehabilitation. A serious undisplaced sprain will be immobilized between 30 and 45 days + 15 days of rehabilitation. A severe sprain with displacement will be operated + 30-day post-operative cast + 15-day rehabilitation. In case of inadequate support, the column of the thumb will not be functional.
7/ SPRAINS OF LONG FINGERS (IPP and IPD)Long finger sprains are injuries of the collateral ligaments of the PIP (proximal interphalangeal) and IPD (distal interphalangeal) which provide lateral stability and are composed of a main ligament stretched in flexion and a stretched accessory ligament in extension.
There is also a cartilage fibro anterior to the volar plate which provides stability to the PIP. It is a powerful palmar ligament inserting on the base of P2 and moving backwards to end in 2 horns on the latero-palmar faces of P1.
Clinical diagnosis is easy: most often swelling of the PIP. Frontal and profile X-rays, or even dynamic X-rays, will specify the possible existence of a bone fragment or radiological laxity which will signify the serious sprain. These sprains are benign traumas and therefore most often neglected by the injured who do not respect the medical instructions; also the sequelae of these sprains in the type of painful swelling and stiffness are commonplace and the lasting functional gene is all the more important as the sprain involves the PPI.
The treatment of these sprains, in particular that of serious sprains, is quite delicate so that their management is the responsibility of specialized structures. Indeed the ligament healing lasts 3 weeks, but if one immobilizes 3 weeks, it is the assured articular stiffness. The current trend is to brace the finger for 2 to 5 days then to practice syndactyly with interdigital foam padding with active physiotherapy for 15 days so as to make the finger painless and mobile with return to sport after 3 weeks. Be careful not to confuse these sprains with buttonhole finger due to rupture of the median strip of the extensor apparatus of the fingers.
Palmar Plate SprainsWhen the finger turns upside down (hyperextension lesional mechanism), it is the palmar plate which is injured and requires more delicate treatment. These palmar plate sprains can lead to a swan neck deformity.
Clinic: hematoma, oedema, pain, major functional impotence.
X-rays: palmar bone tearing.
8/ JUMPING FINGERS
Trigger finger corresponds to a palpable nodular tendinopathy of the flexor tendon next to the metacarpophalangeal pulley. It is found in sports with a strong grip (tennis, golf, rock climbing).
The nodule hangs during the transition from flexion to extension of a finger and can be cured by elective infiltration of the nodule with 1 cc of hydro cortancyl which can be repeated. In case of failure of medical treatment, surgical treatment will excise the pulley with gentle mobilization the day after the operation.
The trigger finger = palpable nodule of the flexor tendon next to the metacarpophalangeal pulley.
9/ RUGBY FINGER or JERSEY FINGER of the FOURTH FINGER
Lesion often diagnosed with delay, the rugby finger corresponds to rupture of the median band on P2 .
It is a lesion that we encounter a lot in the practice of rugby when the jersey grabs on a player who takes his opponent on the wrong foot; the latter then trying to hang him violently by his shirt. This breaks the insertion of the deep flexor tendon (FCP) which will retract on the 3rd phalanx (P3) of the 4th finger.
This 4th finger has a low independence of flexion which does not allow letting go immediately when the 3rd and 5th fingers are flexed, the 5th letting go first.
In addition, the insertion on P3 of the deep common flexor is fragile at the level of the 4th finger because of the lumbricals of the 4th finger uniting with those of the 3rd and 5th.
The clinic is evocative: palmar hyperalgesic swelling of P3 of the 4th finger corresponding to the stump + or - low located depending on whether or not the lesion involves a bone fragment with delayed bruising and impossibility of actively flexing P3 positioned in extension to block the action of the tendon flexor superficial (FCS), while active flexion of P2 is possible (intact FCS). Lateral radiographs should look for distal bone avulsion.
The processing must be done as soon as possible; it is complex and requires a specialized department and will most often be surgical with refixation on P3 of the ruptured tendon with subsequent rehabilitation.
distal tendon rupture of the flexor digitorum profundus muscle of the fourth finger
10/ LESIONS OF THE EXTENSION APPARATUS OF THE FINGER a/ Mallet finger (mallet finger) The mallet finger corresponds to the rupture of the terminal portion of the extensor apparatus of the fingers, here in this case the tendon of the common extensor which is inserted on the dorsal part of the 3rd phalanx (P3).
rupture of the end of the common extensor
The mechanism of injury is a direct distal contusion in forced flexion, for example in ball sports (handball, volleyball), especially on the 4th and 5th fingers; the thumb being very rarely affected.
Diagnosis may be delayed if medical treatment is not immediate and we then find ourselves faced with a P3 extension deficit of the injured finger with irreducible distal flexum.
irreducible distal flexum
As always, lateral X-rays seek to highlight a dorsal bone fragment and make it possible to differentiate between 3 types of lesion of increasing severity depending on the angle of extension deficit:
1- angle less than 30° if incomplete rupture; greater than 30° in the event of total rupture and without bone lesion
2- little displaced distal bone lesion which will be reducible or not in extension
3- displaced bone lesion with subluxation of P3 corresponding to an articular fracture.
The treatment must be done in a specialized environment and will be either orthopedic for 6 weeks by splint or surgical + splint.
b/ Gooseneck deformation: The swan neck lesion corresponds to an inefficiency of the lateral strips which are inserted on the back of P3 and are joined by the lumbrical muscles which pass behind the axis of the phalanx.
The swan's neck very often follows a Mallet finger which is perpetuated.
The deformity increases the Mallet and results in a flexum of the distal phalanx P3 and a hyperextension of the 2nd phalanx P2.
The care comes from a specialized environment.
flexum of P3 + hyperextension of P2
c/ Buttonhole deformation The lesion in buttonhole corresponds to a rupture of the median strip which is inserted on the base of P2 by lesional mechanism in brutal hyper-flexion of the 2nd phalanx P2 which one meets in the sports of varape at the climbers positioning their fingers in arch. The deformation results in a flexum of the proximal interphalangeal (IPP) and a hyperextension of the distal interphalangeal (IPD) and the metacarpo-phalangeal (AMP). Treatment that is difficult to treat is the responsibility of a specialized environment.
rupture of the median band of P2



























Aucun commentaire:
Enregistrer un commentaire